Prednisone and Prednisolone
 Prednisone, known by the brand name Deltasone, and Prednisolone (brand name Orapred, Millipred) are potent immunosupressant, synthetic corticosteroids. They are effectively used to control acute flares in Crohn’s disease. To understand how these medications work, a quick biology lesson is in order.
Prednisone, known by the brand name Deltasone, and Prednisolone (brand name Orapred, Millipred) are potent immunosupressant, synthetic corticosteroids. They are effectively used to control acute flares in Crohn’s disease. To understand how these medications work, a quick biology lesson is in order.
The adrenal cortex is part of the adrenal glands, which are located on the top of each kidney. The adrenal cortex is critical because it produce hormones that flow into the blood stream and affect many different processes in the human body. All hormones produced by the adrenal cortex are steroids derived from cholesterol. The adrenal cortex produces three different classes of hormones:
- Mineralocorticoids, like aldosterone, regulate the salt and water balance of the body which is responsible for blood pressure and making sure we don’t get too dehydrated.
- Glucocorticoids, like cortisol, regulate metabolism and the stress response, and are powerful anti-inflammatory hormones.
- Adrenal Androgens, like DHEA (the precursor to estrogen) and testosterone, are what come to mind for most when the term “steroid” is used, and are responsible for puberty and gender differences.
The corticosteroids which are prescribed in Crohn’s disease are hormones in these first two classes, and do not include adrenal androgens. Prednisone and prednisolone are primarily glucocorticoids, but may have some mieralocorticoid action. They are made synthetically in a laboratory. Because severe inflammation is common in Crohn’s disease, hormones that regulate inflammation were one of the first treatments investigated.
Arthur Nobile, an American microbiologist, was the first to isolate and identify prednisone and prednisolone in 1950. By 1955, working for the Schering Corporation, he and his coworkers had created a commercially feasible drug that was approved by the FDA. Now, both prednisone and prednisolone are available as generic medications from many manufacturers. Prednisolone is on the World Health Organization’s Model List of Essential Medicines.
Prednisone vs. Prednisolone
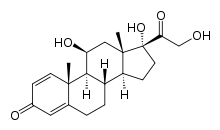
Prednisone is the precursor to prednisolone. When ingested, prednisone is converted to the active, useful form of the medication called prednisolone by the liver, which is more readily absorbed. Prednisolone can be used in patients who have liver failure. While prednisone is usually given orally, prednisolone can be given orally, topically or intravenously. Their chemical structure is slightly different, but their overall mechanism of action and the side effects are the same since the body converts prednisone into prednisolone.
Going forward, this article will use the term “prednisone” to include both medications, unless specified.
Uses and Mechanism of Prednisone
In addition to Crohn’s disease, prednisone is used to treat many other conditions such as lupus, rheumatoid arthritis, multiple sclerosis, asthma, Addison’s disease, allergies and skin conditions. Prednisone works by mimicking the effects of the hormones produced naturally by the adrenal glands to suppress the immune system, but has a much more powerful effect than the naturally occurring hormones. Prednisone suppresses not only the immune response, but the inflammatory products as well. This makes it a valuable, fast acting medication and many patients see an improvement in symptoms within days of starting treatment.
Because this medication is generally systemic (not localized to a specific region in the body) side effects of prednisone can be more severe. Health care providers try to limit the use of prednisone to resolve acute flare-ups and to achieve remission in a short duration. Since prednisone is not very effective at keeping patients in remission or for mucosal healing, it’s not recommended as a long term, maintenance therapy. When prednisone is given for more than 7 days, the adrenal glands begin to stop production of the naturally occurring corticosteroids. Therefore, patients who take prednisone for longer periods must slowly decrease their dosage at the direction of their doctor to allow their adrenal glands time to begin producing the naturally occurring hormones. Stopping prednisone abruptly may lead to a medical emergency called Addison’s crisis, which results from adrenal hormone insufficiency and can be life threatening.
 Generally administered as an oral pill, prednisone as used for Crohn’s disease can also be administered in liquid, injectable, intravenous, topical and rectal forms as well. Adult patients generally begin at a daily dosage of 40-60 mg. for 1-4 weeks until they show improvement or remission. Once the patient is stable, the daily dosage is decreased by 5-10 mg. per week until the patient reaches a daily dose of 20 mg. From there, the taper is slower, decreasing prednisone by 2.5-5 mg. per week until the treatment is discontinued. Patients should be carefully monitored by their health care provider while on prednisone, and side effects should be quickly addressed. The majority of Crohn’s disease patients will initially respond positively to prednisone, but 20-30% will have no response.
Generally administered as an oral pill, prednisone as used for Crohn’s disease can also be administered in liquid, injectable, intravenous, topical and rectal forms as well. Adult patients generally begin at a daily dosage of 40-60 mg. for 1-4 weeks until they show improvement or remission. Once the patient is stable, the daily dosage is decreased by 5-10 mg. per week until the patient reaches a daily dose of 20 mg. From there, the taper is slower, decreasing prednisone by 2.5-5 mg. per week until the treatment is discontinued. Patients should be carefully monitored by their health care provider while on prednisone, and side effects should be quickly addressed. The majority of Crohn’s disease patients will initially respond positively to prednisone, but 20-30% will have no response.
Prednisone is commonly used in pediatric cases, though great care must be taken due to the frequency of adverse affects, as discussed below. The initial dosage is determined by weight, usually beginning at 1-2 mg/kg of body weight, with a maximum of 40-60 mg. daily for 2-4 weeks. (For example, for a 60 lb. child the initial dose would be 27-54 mg. per day. A pound is about .45 kg.) The taper is similar to the adult dose, with a slow taper to discontinuation over an 8-10 week period. For a general overview of traditional treatments in pediatric cases, including prednisone, please see the 2015 research article Current Therapy of Pediatric Crohn’s Disease.
Prednisone Dependence
 Some Crohn’s disease patients (up to 50%) become dependent on prednisone. Steroid dependence occurs when prednisone initially works well to control the Crohn’s disease symptoms, but disease quickly recurs when the patient attempts to decrease the dosage and wean off the medication. Since long term usage of prednisone is discouraged due to side effects, some doctors will attempt to begin a different therapy at the same time the dose of prednisone is slowly tapered down. The hope is that the new therapy will control the patients symptoms and allow them to transition off of the prednisone to a medication with less long term side effects. Unfortunately, some patients have a recurrence of symptoms as the prednisone is tapered down, regardless of concurrent treatment with another medication.
Some Crohn’s disease patients (up to 50%) become dependent on prednisone. Steroid dependence occurs when prednisone initially works well to control the Crohn’s disease symptoms, but disease quickly recurs when the patient attempts to decrease the dosage and wean off the medication. Since long term usage of prednisone is discouraged due to side effects, some doctors will attempt to begin a different therapy at the same time the dose of prednisone is slowly tapered down. The hope is that the new therapy will control the patients symptoms and allow them to transition off of the prednisone to a medication with less long term side effects. Unfortunately, some patients have a recurrence of symptoms as the prednisone is tapered down, regardless of concurrent treatment with another medication.
Side Effects of Prednisone
Severe side effects can occur when taking prednisone including:
- Mood changes: aggression, anxiety, agitation, depression, irritability, nervousness, trouble thinking, insomnia.
- Increased blood sugar levels, particularly for diabetics.
- Steroid-induced Cushing’s syndrome, characterized by a rounded, moon-face, high blood pressure, weak muscles and bones, weight gain, fragile skin that bruises easily and chronic fatigue.
- Susceptibility to infection due to immunosupression.
- Steroid-induced osteoporosis or brittle bones. This can be of particular concern in pediatric case when patients are growing and adding to bone mass.
- Abdominal pain and ulcers, nausea, vomiting.
- Cardiovascular events in children.
- Steroid dependence.
- Vision changes, blurry vision, cataracts.
Less serious, more common side effects of prednisone include:
- Acne or skin rash.
- Increased appetite and thirst.
- Hyperactivity
- Nervousness
- Leg cramps.
- Menstrual abnormalities.
For complete information on prednisone and prednisolone, please see the U.S. National Library of Medicine website.
Potential Interaction of Prednisone (steroids) and MAP
 The argument has been made that a mycobacteria (MAP) could not be involved in the pathology of Crohn’s disease based on the positive response of Crohn’s disease patients to steroids. Critics argue that any therapy which is a powerful immunosuppressant, such as prednisone, should make Crohn’s disease worse if it were caused by MAP, since prednisone would allow for uncontrolled growth of MAP by suppressing the immune system. Therefore, because steroids work so well for many Crohn’s disease patients, a pathogen model of disease must fail. But it’s clear that all traditional therapies have some type of immunosuppressive effect, so more must be at work in the pathology of Crohn’s disease.
The argument has been made that a mycobacteria (MAP) could not be involved in the pathology of Crohn’s disease based on the positive response of Crohn’s disease patients to steroids. Critics argue that any therapy which is a powerful immunosuppressant, such as prednisone, should make Crohn’s disease worse if it were caused by MAP, since prednisone would allow for uncontrolled growth of MAP by suppressing the immune system. Therefore, because steroids work so well for many Crohn’s disease patients, a pathogen model of disease must fail. But it’s clear that all traditional therapies have some type of immunosuppressive effect, so more must be at work in the pathology of Crohn’s disease.
Consider this explanation from Dr. Roderick Chiodini’s article, Crohn’s Disease and the Mycobacterioses: a Review and Comparison of Two Disease Entities.
” The use of steroids in Crohn’s disease and other immunosuppressive therapy are considered contraindicated in pulmonary tuberculosis, exacerbating the disease. However, the detrimental effects of immunosuppressive drugs on mycobacterial infections are not as pronounced as believed. Steroids in combination with antimicrobial agents have been used for treatment of leprosy and in tuberculosis and other mycobacterial infections …. Studies in cattle with paratuberculosis have shown that massive corticosteroid administration does not significantly [negatively] influence the clinical manifestations or outcome of the disease, although it was expected to. Treatment of experimental M. paratuberculosis infection in rabbits with methotrexate, a powerful immunosuppressive drug, resulted in clinical improvement even though the bacillary load increased. In Crohn’s disease, as in tuberculosis and leprosy, steroids are used to provide clinical relief, but neither disease can be cured by such treatment.”
One 2008 study looked at the presence of MAP DNA in patients who were treated with traditional Crohn’s disease therapies vs. controls. The hypothesis was that MAP is detected in few Crohn’s patients because the traditional treatments for Crohn’s disease have also unknowingly been killing MAP as well as reducing inflammation. The study stated that treatment with steroids (including prednisone) had no effect on the presence of MAP DNA in patient’s blood samples, which led the researchers to conclude that steroids will not kill MAP, and treatment with steroids in Crohn’s should be used in conjunction with Anti-MAP therapy. The study has its limitations, and the authors freely admit that the presence of MAP DNA as measured in the study does not equate to viable MAP cultures.
There is one published study which directly examined the effect of prednisone on MAP in vitro. In 2013, a group of researchers examined 342 blood samples from patients with Crohn’s disease, Ulcerative Colitis and healthy controls. Previous studies had found higher antibody levels to a MAP specific protein (PtpA) in Crohn’s disease patients than in controls, which seems to indicate that the immune system is fighting a MAP infection. The researchers hypothesized that standard Crohn’s disease treatments could have some MAP killing effect, and measured the patient’s antibody levels in light of each treatment. Indeed, they found lower antibody levels in Crohn’s disease patients treated with azathioprine. However, the antibody levels of Crohn’s disease patients treated with 5-ASA or steroids (including prednisone) did not decrease. This indicates that prednisone does not affect the growth of MAP in vitro. In fact, the article suggests that steroids may even provide MAP with the building blocks necessary for growth. Therefore, any benefit derived from the use of prednisone in Crohn’s disease is likely not due to its ability to kill MAP, which may explain why prednisone is not curative of Crohn’s disease.
