Crohn’s Disease vs. Ulcerative Colitis
Obtaining the initial diagnosis of Crohn’s disease vs. ulcerative colitis can be difficult. A new research study has found that 44% of Crohn’s disease patients need 10 or more visits prior to their initial diagnosis, and 59% of patients will see 3 or more health care providers during that period of time.
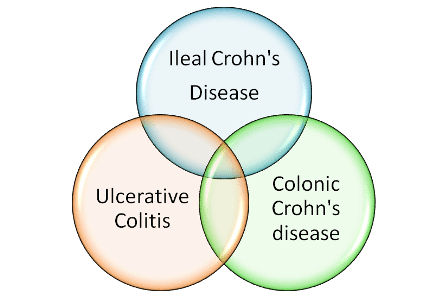
One of the complications in obtaining the initial diagnosis is distinguishing between Crohn’s disease vs. ulcerative colitis. Additionally, 2016 research has identified two sub-types of Crohn’s disease which are independent of age and past treatments:
- Ileal Crohn’s disease – colon tissue resembles a pattern of gene expression commonly seen in the ileum (small intestine).
- Colonic Crohn’s disease – colon tissue resembles a pattern of gene expression commonly seen in normal colon tissue. This subtype is more likely to have severe disease.
10-15% of patients are classified as having indeterminate colitis, which means that their disease has characteristics of both Crohn’s disease and ulcerative colitis.
There are some genetic, histological and symptom overlap between these two diseases. However, the treatment pathway is quite different. While surgery can cure ulcerative colitis, it is only indicated in Crohn’s disease as a last resort. Many Crohn’s disease patients have been mistakenly diagnosed with ulcerative colitis, leading to the removal of their colon, only to have symptoms recur and have their diagnosis changed. It is therefore critical for the health care provider to make the correct diagnosis initially.
The following chart can assist in distinguishing between Crohn’s disease and ulcerative colitis:
| Crohn’s disease | Ulcerative Colitis | |
| Where is the disease located? | Anywhere in the GI tract | The large intestine (colon) |
| Can affect all layers of the bowel wall. | Affects the inner most layer of the bowel wall (mucosa). | |
| Patchy, non-continuous sections of disease mixed between healthy tissue. | Continuous inflammation | |
| Rectal involvement is nearly always present. | Rectal involvement is less common. | |
| Disease is commonly located in the terminal ileum. | Terminal ileum involvement is rare. | |
| Perianal involvement common. | Perianal involvement rare. | |
| Symptoms | Fatty, oily or porridge-like stools. | Stools often contain blood or mucous. |
| Less common feeling of incomplete defecation. | Frequent feeling of incomplete defecation. | |
| The presence of fistulae. | Fistulae seldom occur. | |
| Weight loss is common. | Weight loss is less common. | |
| Risk Factors | Smoking is a significant risk factor. | Smoking is not a risk factor, and may be protective. |
| Peak between ages 15-25. | Onset between 15-30. | |
| Blood Testing | Positive for Anti-Saccaromyces cerevisiae antibodies (ASCA). | Positive for anti-neutrophil cytoplasm antibodies (p-ANCA). |
| Lower platelet-activating factor (PAF) markers. | Higher platelet-activating factor (PAF) markers. | |
| Endoscopic findings | Ulceration is snake-like and can extend into deep tissues. | Ulcers are superficial. |
| Narrowing of the intestine and stricturing. | Narrowing and strictures are rare. | |
| Granulomas present. | The presence of crypt abscesses without granulomas. |
